The process of recuperating from a stroke can be mentally taxing and deeply personal which varies from person to person. The impact of a stroke can be far-reaching, affecting everything from mobility and coordination to cognition and communication. The prognosis for recovery is influenced by a multitude of factors, including the extent and location of the lesion or tissue involvement, as well as the timeliness of treatment, and individual characteristics. Despite these variations, medical professionals have outlined a general progression of motor rehabilitation following a stroke. In this blog, we’ll delve into these Brunnstrom’s stroke recovery stages and what one can anticipate during the stroke rehabilitation stages.
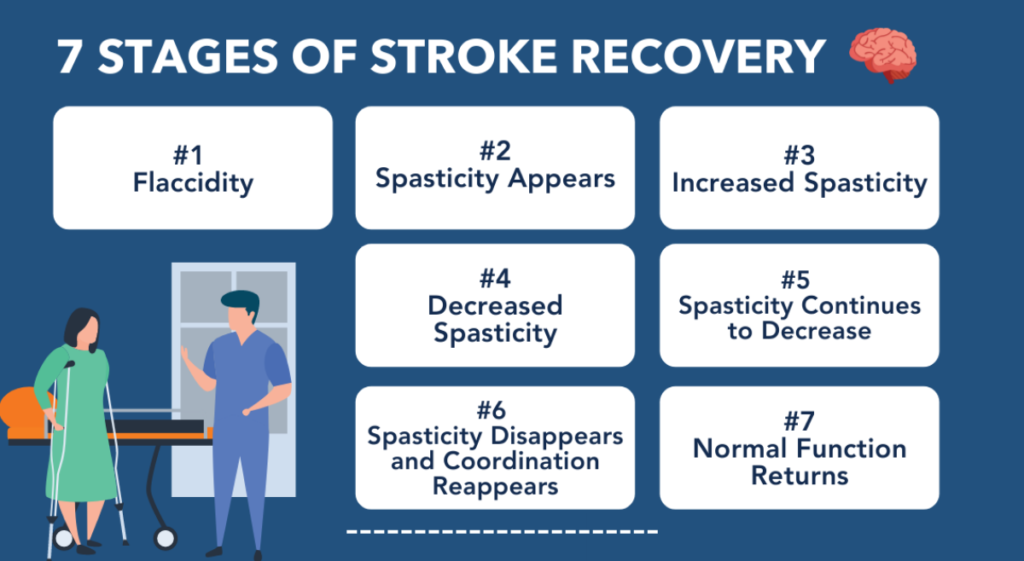
Brunnstrom’s stroke recovery stages
Brunnstrom’s different stages of stroke recovery consist of seven frequently observed phases in the recuperation of motor functions after a stroke, including:
1. Flaccidity
Flaccidity is the initial stage of stroke recovery, occurring immediately after a stroke. During this phase, muscles may be weak, limp, or even unresponsive, giving the impression of being “floppy.” Since a stroke often affects one side of the body more than the other, this flaccidity may be restricted to only one side. It is also common for individuals to experience more severe symptoms in their upper limbs or hands compared to their lower limbs.
Flaccidity is a result of damage to the brain from a stroke. This damage impairs the brain’s ability to transmit messages to particular areas of the body, resulting in limited mobility. Prolonged flaccidity can lead to a significant loss of muscle mass and strength, making it critical to initiate rehabilitation as soon as possible.
2. Spasticity Appears
The second phase of post-stroke recovery stages involves the emergence of spasticity, which is characterized by muscle stiffness and rigidity. During this phase, your limbs may stay contracted, typically in a “flexed” position, with the elbow and wrist bent, or they may shake or tremble when you attempt to move them. While some voluntary movement may return at this stage, it may be limited.
Spasticity is a sign of the brain’s initial efforts to rebuild connections with the muscles, making it a positive indication. However, the connections may be incomplete, causing muscles to become “stuck” in contracted positions or move in unexpected ways. Due to spasticity, it may be more challenging to move your affected limbs, but it is crucial to continue moving as much as possible. This can prevent learned non-use and increase the likelihood of recovery.
3. Increased Spasticity
As you progress into the third stage of stroke recovery phases, you may notice that spasticity, or muscle stiffness, becomes even more pronounced. It can be frustrating to feel like you’re not making progress, but this is actually a sign that your brain is continuing to heal and rebuild connections with your muscles.
It’s important to stay dedicated to your therapeutic exercises during this stage, as they will help you improve your active movement and make the most of your recovery. If you’re still struggling with spasticity, your healthcare provider may recommend Botox injections to help reduce muscle stiffness and maximize your movement during stroke recovery therapy.
4. Decreased Spasticity
As you enter the fourth stage of the stroke recovery process, you’ll likely notice a big shift as spasticity begins to decrease. This is an exciting milestone and a sign that your body is continuing to heal and rebuild. Furthermore, you may also notice improved voluntary movement patterns, although they may still feel jerky, twitchy, and uncoordinated. It’s important to stay patient and continue with your therapeutic exercises during the stroke recovery timeline, as your brain is still working hard to rebuild connections and improve your movement.
5. Complex Movement Combinations
As an individual progresses to the fifth stage, they reach a point where they can seamlessly coordinate complex movements with ease. This could involve the intricate process of picking up a spoon, filling it with food, moving it to their mouth, bringing the spoon back to the table, and then letting go. With the refinement of voluntary movement and coordination, the person gains greater autonomy in performing tasks that are essential for their daily living.
6. Spasticity Disappears & Coordination Reappears
As you progress to the sixth stage of your rehabilitation journey, you’ll likely notice a significant reduction in spastic movements. With spasticity all but gone, your coordination will have improved greatly, allowing you to tackle more complex movement patterns with ease. Now is the time to shift your focus to practicing and refining your coordination and fine motor skills. Take advantage of this stage to work on retaining the more challenging functional activities that you may have struggled with before, such as meal prep, cooking, cleaning, and pursuing your hobbies.
7. Normal Function Returns
After a long and challenging journey through rehabilitation, reaching the seventh and final stage is a significant achievement. It’s a moment when hard work, dedication, and perseverance pay off, and the ultimate goal is realized. At this stage, the patient’s abilities are fully restored, and with the help of elder care service, they can perform complex, coordinated, and synergistic movement patterns on their affected side just as well as on their unaffected side.
However, not everyone reaches this advanced recovery stage. But even if the patient doesn’t reach the ultimate goal, the rehabilitation process can still provide significant improvements in their quality of life, function, and independence. Each step forward is a step in the right direction, and each victory, no matter how small, should be celebrated.
Conclusion
Recovery from a stroke is a highly individualized process, but there is a general pattern of motor recovery that experts have identified. Brunnstrom’s seven stages provide a useful framework for stroke recovery stages, from flaccidity to normal function, detailing the progress of motor recovery following a stroke. These stages help guide rehabilitation and recovery efforts.
Frequently Asked Questions
1. What role does rehabilitation play in stroke recovery?
Rehabilitation plays a crucial role in stroke recovery by helping individuals regain lost skills and abilities through stroke recovery exercises, therapies, and training to improve their quality of life and independence.
2. How long does each stage of stroke recovery last?
The length of stroke recovery stages varies for each individual, depending on the severity of the stroke and the extent of rehabilitation. It can take weeks, months, or even years.

Mahammad Zikriya D
A highly skilled and compassionate Physiotherapist with a passion for patient care and rehabilitation. As the Physio Lead, he brings extensive expertise in assessing and treating a wide range of musculoskeletal and neurological conditions. With a patient-centered approach, I strives to empower individuals to achieve their optimal physical function and quality of life.

